Archive for the ‘mental illness’ Category
November 14, 2009
Lately, I’ve been reading Dr. Drew’s latest book, “The Mirror Effect.” It addresses celebrity narcissism and the extreme behavior that goes along with it. Dr. Drew does a great job at highlighting what has become typical tabloid material – multiple stints in rehab, sex tapes, drug use, eating disorders, etc. – and explaining the self-destructive pathology behind it.
Dr. Drew references troubling celebrity behavior over and over throughout the book. As I read, I found that most responses to this self-destructiveness fit in one of three categories (depending on one’s own background):
3 responses to troubling celebrity behavior:
- Dr. Drew (empathetic / sympathetic)
- “Regular” society (intrigued)
- Relaters (Individuals with their own psychopathology)
The Dr. Drew Response
“As a group, however, [celebrities] often behaved in ways that unnerved and puzzled me.”
“…their behavior makes my heart ache for them.”
I’m coining this the Dr. Drew Response since I can’t think of any other word to better describes the reaction. His heart aches! He sees someone being self-destructive and he cares and feels their pain. It’s sympathy + knowledge + understanding + insight.
“Regular” society
“…this kind of behavior is portrayed as tragically glamorous, dramatically alluring, and, most alarmingly, normal and expected.”
A lot of people are interested in the self-destructive behavior of celebrities. It is a little bit of an obsession: Is Nicole Richie losing weight? Is Lindsay using? Is Amy Winehouse still alive? People want to know. The troubling behavior is intriguing and the press does a great job at, in essence, kicking celebrities when they’re down.
Relaters
“Witnessing such behavior also tends to provoke our own narcissistic impulses, causing us to feel envy, and tempting us to act like the celebrities we admire.”
“But for anyone who has experienced childhood trauma – the fundamental source of pathological narcissism – surrendering to such impulses can lead even mildly narcissistic people to spiral out of control with devastating results.”
Individuals with their own psychopathology or traumatic histories can be tempted (or even feel envious) by the self-destructive behavior of celebrities. There’s something triggering about it that makes these people want to engage in the same self-destructive behavior.
So there we go: In this world we have Dr. Drews, Regulars, and Relaters. I think that your response can change depending on the situation, and that it applies to anyone struggling – not just celebrities.
For example, I think about this girl who went to my college and was very obviously struggling with an eating disorder. “Regular” people would gossip about how sick she was. You’d hear the “I see her at the gym every single morning” and “I heard she eats a plate of broccoli for dinner” comments. Yes, it’s wrong and mean, but unfortunately that’s reality (at least on college campuses). Now, I was a Relater (struggling with an ED myself), so this girl kind of triggered me. I didn’t want to be that sick, but seeing her around campus would almost encourage my eating disorder; tempt me to cut corners, lose just 5 lb., eat a plate of broccoli for dinner, etc. That drove me CRAZY. I didn’t want to be a Relater – I wanted to be a Dr. Drew. I wanted to just empathize with her, wish she would get help, recognize how miserable she probably felt, and know how tough things were for her right now.
This is still a goal of mine: That Dr. Drew Response.
Tags:addiction, addictions treatment, Anorexia, bulimia, celebrity behavior, celebrity narcissism, celebrity psychopathology, childhood trauma, Dr. Drew, eating disorder, mental health, mental illness, narcissistic impulses, pathological narcissism, psychopathology, self-destructive behavior, the mirror response
Posted in Dr. Drew, mental illness, Pop Psych, ptsd | 1 Comment »
June 22, 2009
I read this post on Dads and Daughters With Eating Disorders: Eating Disorders – Weights & Scales
To summarize:
Because her health is directly related to her weight. Measured by scales.
Her recovery is directly related to her weight. Measured by scales.
Her life is directly related to her weight. Measured by scales.
Weight matters.
And scales matter because they measure weight.
I posted a comment on this post, which hasn’t been approved yet, but I decided that I wanted to discuss the issue on Grey Thinking anyway.
Yes, weight is inexorably tied to health and to recovery. Weight restoration is vitally important to recovery. You can’t be recovered and still be below the healthy weight range. Professionals need to monitor weight. Some treatment decisions need to be made based on weight. In short, I am not at all arguing that weight is unimpotant for recovery.
With all of that said… I find a lot of diagnostic criteria and treatment approaches to be contradicting and frustrating. In therapy, you’re told that you are not a number. That you are lovable regardless of what the number on the scale says. That coping with food / weight is not okay. That eating should be mindful and emotional eating is unhealthy. You don’t have to be sick to deserve care.
But think — how is your health measured?
- weight, BMI, % of IBW
- calories, exchanges, % of meal plan completed
- heart rate, blood pressure, potassium, electrolytes
- # of binges / purges, # of laxatives, # of diet pills
- hours exercised
… see my point? Everything is measured in numbers.
I have an issue with your mental health being measured in numbers. From this point of view, gaining weight = a good week and losing weight = a bad week. That has just never been a linear relationship for me. I have bad weeks and gain weight, and vice versa. Sometimes I follow my meal plan and lose weight, and other times I restrict and gain weight. The system reinforces the necessity of communicating through your eating disorder. If you’re feeling crappy but follow your meal plan, then obviously you weren’t really feeling bad — if you were, you would have restricted. Plus, when you are at a healthy weight — ta da, end of treatment! You’re all better! Even if you feel as crappy as ever, you’re not sick anymore, so…..
Thankfully not all professionals practice this way, but measuring your progress in recovery by numbers is not unusual. I feel strongly that weight is just a piece of the puzzle… and while weight and eating are core components to eating disorders, by basing treatment on just these factors you are really limiting treatment. There are people who will stay sick because the system inforces that they need to be to get help. And that’s unfair…
Tags:anxiety, catch 22, coping with food, depression, diagnostic criteria, eating disorder, emotional eating, Health, healthy weight, mindful eating, professionals, recovery, scales, therapy, treatment, weight
Posted in blog, eating disorder, mental health, mental illness, therapy, treatment | 8 Comments »
June 12, 2009

Last night I watched all of the “In Treatment” Sophie episodes. I am just engrossed in this show. I feel so connected to the patients and to Paul. I think that they discuss such intimate details that I feel like I am part of some deep relationship. I can relate to a lot of what the patients say, so Paul’s responses are meaningful to me. It’s also funny that I don’t feel comfortable ending therapy at the end of each season. In episode nine of Sophie I was thinking, “No! You can’t go! There are so many things we still need to talk about. I’m not ready to end therapy! I’m still processing things.”
Anyway, one of the things that struck me about Sophie were all of times that she tested Paul. “Testing” is a good word to describe the scenarios. I probably would have looked at it differently had he not used that word. But yes, “testing” is perfect.
I was trying to think if I’ve ever tested my treatment professionals. I’ve definitely never overdosed, threatened to kill myself, or asked my therapist to change my clothing (I felt so awkward even watching that moment)… but the more that I think about it, the more aware I am of how many times I have tested professionals.
For example:
Nutritionist – With my most recent nutritionist, I’ve turned in a couple of really bad days worth of foods logs to see if she would say something (that wasn’t really the reason they were bad, but it’s the reason I turned them in instead of just not writing those days down). If she didn’t say anything, then it meant that my following my meal plan didn’t matter. She passed. Another time when I felt like she was tired of dealing with me, I stopped making appointments. I figured that when she decided that I needed an appointment, she would say something. No such luck — failed that test.
Therapist – Sometimes my therapist assigns me homework. I’ll do it, but don’t bring it up or turn it in during our next session unless she says something. If she doesn’t, that means she doesn’t remember and it doesn’t really matter. She usually fails this test. It’s probably the only test that she fails, though. For months I didn’t tell her much just because I didn’t trust her… I thought she would think I was ridiculous. So, piece by piece I’d tell her little bits of information and watch how she responded. She was concerned and validating and understanding — definitely passed. Another big issue of mine is calling/emailing/anything outside of a session. I just feel like it is not her responsibility to deal with me outside of that hour a week. I am so afraid that I will be too needy or too much and that I will ruin the relationship. She says that it’s impossible to ruin the relationship, but I don’t know. Anyway, I called her one day when I was really upset, and she was there for me and she wasn’t at all annoyed that I called. Pass.
I could go on, but that’s more than enough examples. While I do like the word “testing,” I think that it has a negative connotation. I think that to some degree, it’s a part of therapy — learning to trust the professional. I hate feeling vulnerable and it takes me a long time to open up and trust someone. I have to feel certain that the person isn’t going to hurt me, though. It’s like testing the waters. It’s hard to build trust. I need to reassure myself somehow that this person is going to care and isn’t going to walk away when I actually need her.
Tags:Anorexia, anxiety, bullimia, depression, eating disorder, food log, in treatment, in treatment sophie, mental health, mental illness, nutritionist, psychology, therapist, therapy, trauma
Posted in mental health, mental illness, Personal, treatment, TV | 5 Comments »
May 30, 2009
I know a lot of patients (and professionals) who refer to their eating disorder as “Ed” (E.D.). I’ve always been a little wary of this… it feels weird to name a disorder that I’m struggling with. It makes me feel like I have schizophrenia or DID or something. However, in some ways it helps to thing of the eating disorder as a separate voice. It helps me to separate what I want from what the eating disorder wants.
My dietitian once told me “don’t bring Ed to dinner – leave him at home.” I have this vision of my sitting at a restaurant, with Ed at the end of the table with just a glass of water. Very silly, I know… but for some reason that helps me. Maybe it’s because I am separating the eating disorder from myself.
People with eating disorders are competitive — that’s (one) reason why you have to be careful who you put in groups together. I have some friends who I really like, but feel competitive with or triggered by. It’s easier for me to think of our two Ed’s fighting. We brought them along with us and now they are arguing.
Okay, now it sounds like I have an invisible friend… and usually I don’t think of the eating disorder as “Ed” — but there are certain situations where it’s helpful for me. But, my question is — what does your Ed look like? Do you have a mental image of it? I’m curious to hear how others envision it. I’ll draw mine and post it in the next entry…
Tags:Anorexia, anxiety, art therapy, bulimia, chronic anorexia, depression, drawing, eating disorder, imaginary friend, mental health, mental illness, mental image, psychology
Posted in eating disorder, mental illness | 13 Comments »
March 15, 2009
It’s been a little while since I talked about Celebrity Rehab, but I have been meaning to write about Gary Busey’s “Buseyisms” (by the way, I highly recommend that you watch this — it’s less than two minutes long). Buseyisms are really just made-up acronyms. Backward acronyms, I guess, but you start with the acronym and come up with the meaning to match the letters.
I’m sure you’ve heard these before… like FINE – Frustrated, Insecure, Neurotic and Emotional. Now, look at a few of Gary’s…
Doubt – Debating On Understanding Bewildering Thoughts
Romance – Relying On Magnificent And Necessary Compatible Energy
Fear – False Evidence Appearing Real
Fun – Finally Understanding Nothing
Sober – Son Of a Bitch! Everything’s Real
Fraud – Finding Relevant Answers Under Deception
Faith – Fantastic Adventures In Trusting Him
So, I thought that I would create some of my own, relating to eating disorder treatment. Personally I don’t think they’re useful — I just think that they are amusing. However, since it took me 2+ hours to come up with these couple of Greyisms, I think that they are a little less fun. Anyway, here’s what I’ve come up with:
- Cope – Changing Overwhelmingly Problematic Experiences
- Shame – Sense of Hurt And Malicious Embarrassment
- Fear – Flee Emotions Around Reality
- Want – Wish About Needing Things
- Denial – Dismiss Every Notion Implying Anything Less
- Therapy – Telling Her Everything Rough About Previous Years
- Support – Someone Understanding Pretty Painful and Overwhelmingly Rejecting Thoughts
- Know – Kinda Not an Original Word
So there you go — those are my best Greyisms. If you come up with better ones (which you will surely do), definitely post them!
Tags:acronym, Anorexia, anxiety, bulimia, buseyisms, celebrity rehab, depression, Dr. Drew, eating disorder, gary busey, mental health, mental illness, recovery, sober house, therapy, treatment
Posted in mental health, mental illness, Misc, TV | 3 Comments »
March 11, 2009
There is definitely a stigma surrounding mental illness. It doesn’t receive the same kind of acceptance as physical illness. I’m not really going to get into stigmatization and society and whatnot, but I just want to make it clear that I believe that physical illness is much more understood than mental illness.
That said, I am a little disappointed to read this article on relationships and mental health:
A partner is four times more likely to leave you because of a mental health condition like depression than because of a physical disability.
The survey, which asked people about issues that would make them break off a romantic relationship found that 20 per cent of British women wouldn’t stay with someone if they were diagnosed with schizophrenia, yet only a few of them would break up with someone who became disabled and needed to use a wheelchair.
The article chalks up the entire discrepancy to stigmatization. Naturally, I think that there are other elements contributing to this problem:
- Personality changes – I think the biggest issue is that mental illness has a larger impact on your personality, mood, and temperament. It’s not easy to be around someone who is really depressed. You want to connect with your partner, spend time with them, and in general just be happy to be around them. Most mental illnesses cause people to push others away, be irritable, isolate, etc. These qualities are not very conducive to relationships. In high school, my eating disorder definitely affected my relationships. I didn’t want to go out to eat. I didn’t want to see a late-night movie because I was too tired. I took everything personally and was really depressed. I was much more interested in the disorder than in my relationships. I was not a fun date (to say the least).
- Expectations of recovery – I think that it’s frustrating to be with someone who you feel should be getting better, but isn’t. If you are in a wheelchair (to continue with the article’s example), you might never be expected to walk again. However, if you have an eating disorder, you are expected to get over it. It’s tiring to spend years and years worrying about someone who is continually in and out of treatment, rarely making significant gains in their recovery. Your expectations are different. Realistic or not, it can be exhausting to watch someone chronically struggle and feel like they don’t necessarily even want to get better.
- You don’t know what you’re getting into. When you start dating a guy in a wheelchair, you know he’s in a wheelchair. You very well may not know that your date is bipolar, though. Again, it’s an expectations thing.
- Baggage. As non-PC as this is, it’s true — mental illness carries a lot more emotional baggage than physical illness. Someone with a mental illness is more likely to have a familial history of mental illness, childhood abuse, an alcoholic parent, or some other kind of trauma. Eating disorders don’t develop in a vacuum, right?
Naturally, I wouldn’t discourage anyone from dating someone with a mental illness. Actually, I don’t even like the “mental illness” label. If we’re all on a mental health / mental illness continuum, then where do you draw the line, anyway? (this is a discussion for another time!) I just think that there’s a lot more at play than just stigmatization.
Tags:Anorexia, anxiety, bipolar, bulimia, depression, eating disorder, eating disorder recovery, eating disorder treatment, mental health, mental illness, mental illness stigma, physical disability, relationship, relationships, sociology, stigma
Posted in mental illness, relationships, sociology | 1 Comment »
February 25, 2009
Headline: Bad Economy Spurs Eating Disorders
According to Twin Cities, the patient load at Park Nicollet’s Melrose Institute/St. Louis has increased by 36 percent from one year ago, while the patient load at The Emily Program/St. Paul has increased by 20 percent for the same time period.
For instance, he says, people who suffer from an obsession with their weight, but who exercise to control weight gain rather than starve themselves, may no longer be able to afford their gym memberships. In that case, Jahraus says, they may decide to limit their food intakes, which can lead to eating disorders.
Oh, this article could have been so interesting! It was an interesting thought. The part about not being able to afford your gym membership and therefore developing an eating disorder killed the article (for me), though. Oh well…
Still, I wouldn’t jump to the conclusion that a bad economy spurs eating disorders… but rather that a bad economy motivates more people to get help for their eating disorders. Why is this?
Well, I think that there are several reasons….
- A big barrier to treatment is work. You have responsibilities… you can’t just disappear for a month or two to go into treatment all day. If you are laid off, though, suddenly you are available in the middle of the day. You don’t have another commitment. You have time to get the treatment that maybe you’ve needed for a couple of years but never felt you had time to get.
- Feelings of disappointment, shame, and embarrassment. These are tough feelings for anyone, but are especially tough feelings for someone with an eating disorder. It’s not unlikely for someone with an ED to take being laid off personally… as if they somehow failed. They might think it is a reflection of themselves — they’re not good enough. What are they going to tell friends and family? Others will be so disappointed. When you’re feeling this depressed and hopeless, you’re more motivated to go and get help — you don’t want to feel like this.
- Lack of structure. Many people with eating disorders struggle with endless periods of free time. Work provides a daily structure that’s helpful. When you are missing that, sometimes things fall apart. Maybe getting intense treatment will help you with that transition… to either help you figure out how to cope with the free time or to tide you over until you get a new job.
- Friends and family have time to notice your issues. If you’re at work all day, your friends and family might not realize how little you’re eating or how much you’re exercising. When you’re suddenly at home all the time, they have a much clearer picture of what your eating/exercising habits are like during the day… and they might be concerned and encourage you to get treatment.
Tags:Anorexia, anxiety, bad economy, bulimia, depression, disappointment, eating disorder, eating disorder recovery, eating disorder treatment, emily program, exercise, food intake, mental health, mental illness, psychology, relapse, shame, starve, twin cities, weight gain
Posted in eating disorder, mental illness | 3 Comments »
February 13, 2009
Coloring aside (and other “active meditation,” I guess), there is something that I hate about meditation (guided imagery especially). Deep breathing maybe helps me when I’m starting to freak out, but I think that’s because I’m telling myself “chill, take a moment, calm down, relax, collect yourself, you’ll be okay.” However, breathing deeply does stop my heart from beating so quickly.
Meditation is different though. I think it’s frustrating and I feel so impatient with it. It’s supposed to be calming, but really it just wears on my attention span and my nerves. It’s like when you’re stuck sitting at a red-light in the middle of the night, and are the only car there. You are watching that light and a minute goes by…. another minute… and you start thinking, “Seriously? You have to be kidding.” Another minute goes by and you are convinced the thing is broken. FINALLY the light changes.
I’ve had several therapistic explanations for this:
- I think I am a human doing, rather than a human being.
- I am uncomfortable sitting with myself.
- Meditating is letting my guard down and I am afraid to make myself that vulnerable.
- That’s my eating disorder talking (which I don’t think is really even relevant in this situation, but I swear there are therapists who say this about everything)
I think I can sit with myself and be calm. I love long car rides, coloring, napping, walking the dog… if you don’t count any of these “sitting with yourself and being a human being,” then what else besides meditation fits into this category?
When I am feeling panicky and anxious, meditation is about the last thing in the world that I want to do. It sounds so wrong when you state it this way, but some degree of anxiety is less painful than meditation! I think it’s great that meditation is calming and refreshing for some people… but I am convinced that meditation is not for everyone, and that it’s not necessarily a symptom of mental illness.
Tags:Anorexia, anxiety, bulimia, chronic anxiety, coloring, coping skill, depression, eating disorder, ED recovery, ED treatment, human being, meditation, mental health, mental illness, napping, NEDA, panic attack, someecard, therapist, traffic light
Posted in Health, mental illness | 2 Comments »
January 26, 2009
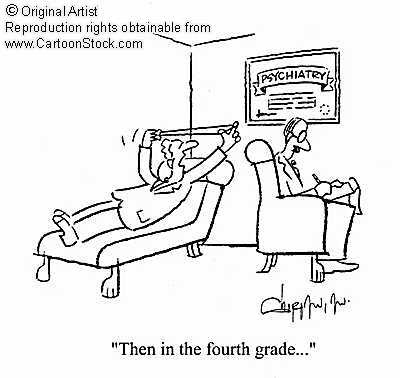
Do you ever feel like this in therapy? You’re talking about something random that happened in your childhood that you’re nearly POSITIVE has nothing to do with your issues today?
For example….
Before kindergarten I got to try out three different schools — and my parents did not send me to the one that I liked! And then I had to play with this girl who my mom was friends with who I did not get along with. Trauma! Oh, and there was this boy in kindergarten who would always kiss me and I hated it. And I finally told the teacher and she didn’t care and told me to deal with it!
Clearly this is the source of my issues with intimate relationships. I’m afraid of letting people in because they might get TOO close and I might not be able to do anything about it. And this teacher reinforced the idea that my feelings do not matter and that the world doesn’t care about what I’m going through. Being made to play with a girl I didn’t like is one of many examples of my parent’s control issues. Maybe even some enmeshment, since they weren’t letting me choose my own friends.
Now, I’m not saying that the past doesn’t matter. It absolutely helps shape you and plays a role in what you’re dealing with today. And everyone is impacted by things differently…. maybe being kissed by that boy would be traumatic for someone else. I am not trying to minimize these events. I have known professionals who want to just start at the beginning of your life and work through the whole thing… and who think that this is necessary for recovery.
What do you think — how much analysis of the past is necessary for ED recovery?
Tags:Anorexia, anxiety, bulimia, cartoon, childhood, depression, eating disorder, eating disorder treatment, fourth grade, memories, mental health, mental illness, psychiatry, psychoanalysis, psychotherapy, recovery, trauma
Posted in eating disorder, mental health, mental illness, Misc | 4 Comments »
January 19, 2009
This is nothing new, but everyone seems to be on some kind of diet. Or, if they’re not “dieting,” then they are eating purely organic food, or only raw foods, or cutting out all white flour and sugar. All of this leads me to ask myself — if this kind of eating is “healthy” or “okay” for the rest of the world, why isn’t it okay for me?
I think that the line between healthy and disordered is so fuzzy (grey territory, I’d say). Eating organic is healthy. Raw foods are healthy. White flour and sugar are not the healthiest ingredients out there. This is how everyone should be eating… right? In ED treatment you’re taught that there are no “bad foods” — there’s that “everything in moderation” idea. And while residential we definitely had cookies, sugar cereal, non-organic fruits and vegetables, non-whole-wheat pasta, etc.
Where’s the line between healthy and too healthy? And if all these people can be so picky about food… obsessing over healthiness… what’s the big deal about my eating disorder? If I ordered a salad sans croutons and dressing (which I would never do — I love croutons.), it would be eating disordered. If my friend did the same, it would be healthy. Why the double-standard?
My mom cooks primarily out of the Weight Watchers cookbook (note: no one in my family has ever done weight watchers nor has really needed to lose weight), because “it’s healthier.” My fiance makes mac & cheese without any butter or milk because “it’s healthier.” Both of these behaviors seem disordered to me (although my fiance does NOT have an ED. At all. My mother’s another story).
I spent so much time arguing with myself about this… and ultimately just had to give up and let the whole issue go. I don’t know where the line is — because actually, the line moves, depending on the person, situation, and a hundred other variables. And really, healthy/unhealthy labels aside, my vision of recovery includes sugar and white flour. I’ll admit to owning the Mayo Clinic’s recipe book — but not Weight Watchers. Even if Weight Watchers isn’t at all disordered and IS the healthier way of doing things — I don’t want it. I plan on making mac & cheese correctly, eating carbs after 9pm, sometimes having more than one glass of wine, and eating the bread that they serve at restaurants… even if “normal” people without a history of an eating disorder insist it’s unhealthy!
One thing I love about eating disorder treatment is that the recovery ideal seems so livable (albeit slightly unbelievable and unattainable). No diet food, no skipping meals, no overworking or over-stressing yourself, moderate exercise (aka: not 60+ minutes a day, every day), 8 hours of sleep, lots of support, time to take care of yourself, etc. Maybe I could technically “recover” and still eat fat-free yogurt, get 5 hours of sleep a night, take on too much responsibility at work and never take a vacation — but do I really want to? (No).
I don’t want to be so preoccupied with food, exercise, and weight forever. If that’s the healthy, “normal” thing to do, then I’m aiming for a different normal — Renfrew-normal (or just ED recovery-normal, although that’s slightly more ambiguous). It sounds like a much more enjoyable existence.
Tags:Anorexia, anxiety, bulimia, depression, eating disorder, eating disorder recovery, ED treatment, food obsession, healthy eating, meal plan, mental health, mental illness, normal eating, organic food diet, raw foods, Renfrew
Posted in Anorexia, eating disorder, mental health, mental illness, Personal | 7 Comments »