Posts Tagged ‘bulimic’
October 17, 2009

It feels a little cliche quoting Grey’s Anatomy on Grey Thinking, but there are so many good quotes…. and I’ve been re-watching the series from the beginning (hey, why not?), and it’s funny how some things stand out to you when watching for the second time.
You’re happy? You’re happy now? The Meredith I knew was a force of nature. Passionate, focused, a fighter. What happened to you? You’ve gone soft! Stammering about a boyfriend and saying you’re waiting to be inspired. You’re waiting for inspiration? Are you kidding me?! I have a disease for which there is no cure, I think that would be inspiration enough! Listen to me, Meredith. Anyone can fall in love and be blindly happy! But not everyone can pick up a scalpel and save a life. I raised you to be an extraordinary human being, so imagine my disappointment when I wake up after five years and discover that you are no more than… ordinary! What happened to you?!
— Ellis Grey, Grey’s Anatomy
Sometimes I look back on my high school years (when I was deep in the ED) and think that I was a better person then. Somehow I seem to think that back then I tried harder, was more earnest, focused, passionate, smarter… and that now I’ve somehow “gone soft.” I’ve failed at being anything “extraordinary.” I couldn’t hack it, I gave in, and I’m really nothing but ordinary.
In reality, I know that I was miserable in high school, completely immersed in the eating disorder and in a fog of depression and hopelessness. There was nothing better about me then. And, the anorexia did not make me extraordinary. It did not make me special. It made me sick, sure… but heck, the flu makes you sick. Water in Mexico makes you sick. Being sick doesn’t make you extraordinary. It just makes you… sick.
I don’t think it’s uncommon to dislike the idea of being ordinary. Ordinary to me means… unmemorable, unimportant, unremarkable, unexceptional, and lots of other un- words. You don’t want to your life to be of no significance. You want to be memorable and you want to feel like your life matters!
I’ve often said that I still hold on to the eating disorder “just in case.” In case I am a disappointment, in case I can’t measure up, in case I’m not worthwhile. This is so ironic though, because the eating disorder really robs you of so many things in your life. The more involved I am in the ED, the less present I am in the rest of my life. I’m less focused on work, less invested in relationships, and less interested in hobbies or holidays or anything.
I think that eating disorders distance you from everything that makes you extraordinary. They blunt all the things about you that do make you special. And it’s sad (and a little ironic, actually), because some of the most amazing people that I know are friends who I made in treatment
Tags:Anorexia, anorexic, bulimia, bulimic, eating disorder, EDNOS, ellis grey, extraordinary, grey's, grey's anatomy, mental health, mental illness, ordinary, psychology
Posted in eating disorder, TV | 3 Comments »
October 8, 2009
While I do have several new posts on the way, I want to highlight a couple of older Grey Thinking posts (some are several years old! I bet you were not reading GT two years ago) that talk specifically about treatment, your attitude toward treatment, recovery expectations, etc. While there are a couple of people that I have in mind when it comes to the subject of these posts, I think that everyone can use the refresher.
You as your own case manager
Originally Posted: 01/01/2009
I wish that all these guys were going to stay clean, I really do. I’ve just seen it so many times that I can tell when someone’s really willing to do whatever it takes and when someone’s willing to do what they think it should take. And it’s just not going to work like that, unfortunately.
–Shelly, Celebrity Rehab with Dr. Drew 2
Wanting to want to recover
Originally Posted: 06/12/2008
Motivation to change implies an intention–weak or strong–to change one’s behavior. However, AN patients may at the same time both wish to recover and be highly resistant to change their behavior. Therefore, we suggest that assessment of motivation in these patients should include not only their motivation to change, but also their different wishes to recover which do not necessarily imply a behavioral intention.
Dr. Drew should treat eating disorders
Originally Posted: 07/01/2008
There are a lot of components of addiction treatment that I believe in and think are important, and should be applied to eating disorders:
- Recovery is a lifelong, daily process
- Denial, and not necessarily that you have a problem, but that you need help
- The importance of personal accountability
- There’s no magic cure
- The disorder should be taken as seriously as any potential fatal disease
Do not pass Go, Do not collect $200
Originally Posted: 12/09/2008
“I don’t want to play the rehab game anymore”
– Jeff Conaway, Celebrity Rehab 2
I think that recovery can feel like a game at first because it is so different from the rest of your life. It’s nice to have others care about your wellbeing and there’s something about treatment that gives you permission to take care of yourself. Plus, there is so much positive reinforcement (gold star for following your meal plan over the weekend!). All of this doesn’t sound so bad… and I do believe you can make progress — even with this mindset.
When does the game end? Personally, I think this is when the disorder starts to feel threatened. There is something scary about recovering, and suddenly it doesn’t sound like a great idea anymore.
“I don’t want to play the rehab game anymore”
– Jeff Conaway, Celebrity Rehab 2
I think that recovery can feel like a game at first because it is so different from the rest of your life. It’s nice to have others care about your wellbeing and there’s something about treatment that gives you permission to take care of yourself. Plus, there is so much positive reinforcement (gold star for following your meal plan over the weekend!). All of this doesn’t sound so bad… and I do believe you can make progress — even with this mindset.
When does the game end? Personally, I think this is when the disorder starts to feel threatened. There is something scary about recovering, and suddenly it doesn’t sound like a great idea anymore.
Tags:Anorexia, anorexic, bulimia, bulimic, celebrity rehab, Dr. Drew, eating disorder, eating disorder recovery, eating disorder treatment, ED treatment, inpatient eating disorder, inpatient hospitalization, inpatient treatment, jeff conaway, recovery, rehab, sobreity
Posted in Dr. Drew, eating disorder, treatment | 3 Comments »
July 1, 2009
“I’m not deflecting because I’m avoiding something deep. I’m deflecting because I’m avoiding something shallow.” – House, MD
One of my biggest treatment pet peeves is when professionals ask non-deep “deep” questions. For example:
- What does it mean to feel?
- How did it feel to be in that space?
- How does it feel to be in this space now?
- What does it mean for you to not be in that space anymore?
- How do you experience that process?
- What would it mean for there to be grey in your world?
- How does it feel to have acknowledged that out loud?
Okay, depending on the situation, some of these questions could potentially be useful. However, I’ve had therapists who use them over and over and over again. “What does it mean to feel?” is probably my least favorite question of all. Maybe it SOUNDS deep and therapeutic, but there are really only two answers to this question:
- It means that I have feelings
- It means that I am allowed to have emotions and that it’s okay for me to recognize them and not judge them as being either “good” or “bad”but to just accept them as they are… and that emotions may be scary but I can work through them and get support to handle them… and that they are normal and a necessary part of human life and essential to enabling us to connect to other humans and form relationships….
My point is, your answer is either “this is a stupid question” or “I just had this revelation about the significance of feelings and everything else in my life.” And if your answer is the first, then it’s “But what else? What does it really mean?” This is where the House quote comes in. I’m not deflecting the question because I don’t want to address some deep underlying issue, but because it’s really not a deep question! And if you won’t accept “Um, it means that I have feelings” as an answer, then you are going to get whatever fictitious BS I can come up with off the top of my head. Plus, I’ll be frustrated and won’t want to intelligently answer your additional questions.
You can ask me what I’m feeling, what I felt at that time, how I feel about feeling that way, etc…. but I hate when it is reworded to sound like a deep question. “How does it feel to be in this space now?” is just “How do you feel?” with six extraneous words.
Wow, I swear I am not as bitter (or as difficult of a patient) as I sound in this post! I just don’t like shallow questions that are pretending to be deep.
Tags:Anorexia, bulimia, bulimic, chronic eating disorder, deep question, eating disorder, eating disorder recovery, eating disorder treatment, emotions, feelings, psychotherapy, therapeutic, therapist, therapy, treatment
Posted in treatment | 8 Comments »
July 1, 2009
“I’m not deflecting because I’m avoiding something deep. I’m deflecting because I’m avoiding something shallow.” – House, MD
One of my biggest treatment pet peeves is when professionals ask non-deep “deep” questions. For example:
- What does it mean to feel?
- How did it feel to be in that space?
- How does it feel to be in this space now?
- What does it mean for you to not be in that space anymore?
- How do you experience that process?
- What would it mean for there to be grey in your world?
- How does it feel to have acknowledged that out loud?
Okay, depending on the situation, some of these questions could potentially be useful. However, I’ve had therapists who use them over and over and over again. “What does it mean to feel?” is probably my least favorite question of all. Maybe it SOUNDS deep and therapeutic, but there are really only two answers to this question:
- It means that I have feelings
- It means that I am allowed to have emotions and that it’s okay for me to recognize them and not judge them as being either “good” or “bad”but to just accept them as they are… and that emotions may be scary but I can work through them and get support to handle them… and that they are normal and a necessary part of human life and essential to enabling us to connect to other humans and form relationships….
My point is, your answer is either “this is a stupid question” or “I just had this revelation about the significance of feelings and everything else in my life.” And if your answer is the first, then it’s “But what else? What does it really mean?” This is where the House quote comes in. I’m not deflecting the question because I don’t want to address some deep underlying issue, but because it’s really not a deep question! And if you won’t accept “Um, it means that I have feelings” as an answer, then you are going to get whatever fictitious BS I can come up with off the top of my head. Plus, I’ll be frustrated and won’t want to intelligently answer your additional questions.
You can ask me what I’m feeling, what I felt at that time, how I feel about feeling that way, etc…. but I hate when it is reworded to sound like a deep question. “How does it feel to be in this space now?” is just “How do you feel?” with six extraneous words.
Wow, I swear I am not as bitter (or as difficult of a patient) as I sound in this post! I just don’t like shallow questions that are pretending to be deep.
Tags:Anorexia, bulimia, bulimic, chronic eating disorder, deep question, eating disorder, eating disorder recovery, eating disorder treatment, emotions, feelings, psychotherapy, therapeutic, therapist, therapy, treatment
Posted in treatment | 8 Comments »
May 25, 2009
I started this day in a panic over insurance. I hate insurance. I know that is such a blind, ignorant statement, but at this moment (and a lot of other moments) I really do.
Unfortunately it is a holiday (well, that in itself is not unfortunate), which means that neither insurance nor my treatment provider is working. There’s nothing I can do about it today. I can’t resubmit my claim or beg for more days. I don’t know if I will be going to my appointment tomorrow.
I don’t want to spend the next 24+ hours fretting over this, but at the same time, I do want to. I know that worrying is not productive, but my mind is filled with “what if?”s and worst-case scenarios. It’s as if turning it over and over in my mind will somehow prepare me for whatever happens tomorrow.
While trying to remind myself that worrying is not productive, I remembered this quote:
Behind all of this lay the “mind like water” concept … when you throw a pebble into a pond, what does the water do? It responds with total appropriateness to the force and mass of the rock. It does nothing more and nothing less. It doesn’t overreact or underreact. It doesn’t react at all. It simply interacts with whatever comes to it and then returns to its natural state. – David Allen, Getting Things Done
So that’s my goal for today and tomorrow: “mind like water.” I have to let it go for today. I will try and be calm until hit with the insurance rocks.
Tags:Anorexia, anorexic, anxiety, bulimia, bulimic, david allen, depression, eating disorder, getting things done, health insurance, insurance, mental health, mental illness, psychology, ptsd
Posted in anxiety, mental health, therapy, treatment | 2 Comments »
May 24, 2009
I am not an auditory learner. At all. I’m definitely a visual learner — in college I took copious notes, but didn’t really grasp the class material until later going over and reading those notes. There’s just something about reading/writing that I need to get it.
Unfortunately, this doesn’t serve me too well in therapy. I can have a great session and later that night not even remember half of what we talked about. And on the same level, when I’m in session I don’t remember half of what I planned to say.
In an effort to make my time in therapy more useful, I’ve started to write things down. Not quite journal, but write when I’m upset or just a couple of points I want to make sure that I let my therapist know. If I’m afraid that I won’t bring up the issue in therapy, sometimes I’ll email them to her before my appointment.
That’s just one way that writing things down helps me in treatment. Another is with my meal plan. I know my meal plan backwards and forwards at this point, but one day I decided to pin it to pin it to my bulletin board above my desk. This probably sounds silly, but it has made such a difference. I am reminded all day that my meal plan and recovery are important. When I’m in the middle of work I think “oh, I’ll eat that later” or “I am too busy right now,” but just having it written out and sitting in front of me helps me remember that treatment is important even when I’m not in my therapist’s office.
A third way is with affirmations. Well, affirmations may not be the word that I’m looking for… but clips of little things that mean something to me. For instance, also on my bulletin board is a fortune from a fortune cookie that says “Remember there are people who care deeply about you.” I also have this paper on which my therapist wrote, “You can let go of your ED and still be validated” and “Never forget, but forgive and make yourself a better person.” And then, sometimes I’ll print out pieces of funny or significant emails (from anyone in my life) and pin those up. Yes, I have a very large bulletin board!
I need a written reminder for several reasons:
- I’m a visual person
- I twist things and second-guess myself and think “she didn’t mean it that way” or “I am reading into that too much.”
- Being continually reminded helps me convince myself that it is true
Different types of therapy are helpful for different people, and I think that there is some trial-and-error involved in figuring out what works for you. Personally, I highly recommend investing in a bulletin board.
Tags:affirmation, Anorexia, anorexic, anxiety, auditory learner, bulimia, bulimic, bulletin board, depression, disordered eating, eating disorder, eating disorder recovery, eating disorder treatment, mental illness, psychology, recovery, trauma, treatment, types of learning, visual learner, writing
Posted in eating disorder, therapy, treatment | 4 Comments »
May 24, 2009
I am not an auditory learner. At all. I’m definitely a visual learner — in college I took copious notes, but didn’t really grasp the class material until later going over and reading those notes. There’s just something about reading/writing that I need to get it.
Unfortunately, this doesn’t serve me too well in therapy. I can have a great session and later that night not even remember half of what we talked about. And on the same level, when I’m in session I don’t remember half of what I planned to say.
In an effort to make my time in therapy more useful, I’ve started to write things down. Not quite journal, but write when I’m upset or just a couple of points I want to make sure that I let my therapist know. If I’m afraid that I won’t bring up the issue in therapy, sometimes I’ll email them to her before my appointment.
That’s just one way that writing things down helps me in treatment. Another is with my meal plan. I know my meal plan backwards and forwards at this point, but one day I decided to pin it to pin it to my bulletin board above my desk. This probably sounds silly, but it has made such a difference. I am reminded all day that my meal plan and recovery are important. When I’m in the middle of work I think “oh, I’ll eat that later” or “I am too busy right now,” but just having it written out and sitting in front of me helps me remember that treatment is important even when I’m not in my therapist’s office.
A third way is with affirmations. Well, affirmations may not be the word that I’m looking for… but clips of little things that mean something to me. For instance, also on my bulletin board is a fortune from a fortune cookie that says “Remember there are people who care deeply about you.” I also have this paper on which my therapist wrote, “You can let go of your ED and still be validated” and “Never forget, but forgive and make yourself a better person.” And then, sometimes I’ll print out pieces of funny or significant emails (from anyone in my life) and pin those up. Yes, I have a very large bulletin board!
I need a written reminder for several reasons:
- I’m a visual person
- I twist things and second-guess myself and think “she didn’t mean it that way” or “I am reading into that too much.”
- Being continually reminded helps me convince myself that it is true
Different types of therapy are helpful for different people, and I think that there is some trial-and-error involved in figuring out what works for you. Personally, I highly recommend investing in a bulletin board.
Tags:affirmation, Anorexia, anorexic, anxiety, auditory learner, bulimia, bulimic, bulletin board, depression, disordered eating, eating disorder, eating disorder recovery, eating disorder treatment, mental illness, psychology, recovery, trauma, treatment, types of learning, visual learner, writing
Posted in eating disorder, therapy, treatment | 4 Comments »
May 18, 2009
 There have been many blog posts written on facebook and pro-anorexia, however, lately I’ve been thinking a lot about facebook and recovery in general.
There have been many blog posts written on facebook and pro-anorexia, however, lately I’ve been thinking a lot about facebook and recovery in general.
Facebook is really unique in that EVERYONE (okay, almost everyone) is on it. If you’re an eating disorder patient, this means your professionals, the other girls/guys you’re in treatment with, past patients, your school / work friends who may not know about your eating disorder, your family members, etc. In what other realm do all of these people connect?
For most people, “Facebook stalking” means checking out what that guy you liked in high school is doing now (or some variation of that idea). However, for anyone in eating disorder treatment, Facebook stalking can mean following up on the girls you were in treatment with or tracking down all of the professionals you’ve worked with.
Luckily, there are privacy settings. Some professionals even know how to use them.
I was pretty convinced that facebook could be nothing but hurtful to recovery until a girl I used to be in treatment with told me how she and another woman used it to keep in touch. There’s probably a 20-year age difference between the two girls (for the sake of this example, let’s call the older one Kristy and the younger one Jackie), but neither of them had a lot of support outside of their families. In the evenings they would talk on facebook (something I haven’t gotten into yet — facebook messenger). Kristy would see the unhealthy things about dieting that girls would post on Jackie’s wall, with prom coming up, and they’d talk about it. Jackie saw all the cute pictures of Kristy’s kids. Basically, it served as an outlet for both of them — something that was missing in their outside world.
Now, you could argue that this isn’t different than email or IM, but I don’t think that IM bridged the age-barrier in the same way that facebook is now. IM also doesn’t have the public information that facebook has — you can’t see how others interact with someone.
So what do you think about facebook — helpful or harmful to recovery? Staying in touch with people you were residential with could definitely be triggering (especially if they are not doing well and you have access to their photos), but having the support of people who have been great friends is also valuable. And I’d love to know — do professionals ever search for their clients on facebook? Just out of curiosity? For the record, I have never tried to friend a professional myself — although I won’t lie, I have looked at a couple of profiles.
Tags:Anorexia, anorexic, anxiety, blog post, bulimia, bulimic, depression, Dieting, eating disorder, eating disorder treatment, facebook, facebook stalking, inpatient, mental health, mental illness, pro-anorexia, professionals, psychiatry, psychology, ptsd, recovery, relapse, relationships, residential, social media, therapist, trauma, treatment, triggering
Posted in eating disorder, online support, relationships | 14 Comments »
May 15, 2009
 Food rituals are pretty common among individuals with eating disorders… cutting things into tiny pieces, chewing a certain number of time, mixing weird things, eating everything separate, picking food apart, etc. I’ll be the first to admit that I’ve never been terribly successful in eliminating my own food rituals. As I was miserably failing my goal to “eat a bagel normally” this morning, I was thinking about what it was that seemed so necessary about the rituals.
Food rituals are pretty common among individuals with eating disorders… cutting things into tiny pieces, chewing a certain number of time, mixing weird things, eating everything separate, picking food apart, etc. I’ll be the first to admit that I’ve never been terribly successful in eliminating my own food rituals. As I was miserably failing my goal to “eat a bagel normally” this morning, I was thinking about what it was that seemed so necessary about the rituals.
I don’t think that cutting food up changes the calories. I don’t pick things apart because it makes me eat more slowly. I don’t think that eating food with a fork makes it safe. For some reason, though, being able to do the food ritual makes that food manageable. It’s a nervous energy. Not picking the food apart KILLS me (well, or so it feels). I just feel so driven to do it.
So, my question is — where do you draw the line between ED food ritual and obsessive compulsive behavior? Of course the two diagnoses cross paths, but not everyone with food rituals has OCD (and vice versa). Is it a food ritual if you think the action makes the food safe or unsafe? Or if you think that somehow it affects whether or not you gain weight? Or is it only an OCD behavior if you have other OCD behaviors (checking, counting, etc.)? Can you be diagnosed with OCD if you only have food rituals? Is that enough of an obsession/compulsion? And, if your food rituals are more of an OCD issue than an eating disorder issue, do you approach treatment for that differently?
I’d love to hear your thoughts on this!
Tags:Anorexia, anorexic, anxiety, bulimia, bulimic, depression, diagnosis, eating disorder, food rituals, irrational beliefs, mental health, mental illness, obsession, obsessive compulsive, OCD, psychology, recovery, relapse, treatment
Posted in diagnosis, eating disorder, OCD | 16 Comments »
May 9, 2009
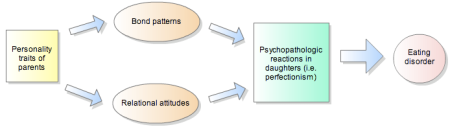
There have been many studies on family dynamics and the development of eating disorders, but I think that this is the first that I’ve seen that takes the next step and makes connections with specific symptomology: The dynamic relationship of parental personality traits with the personality and psychopathology traits of anorectic and bulimic daughters
Before I go further, I want to make two disclaimers. First, from the article:
…we cannot infer a casual relationship between the parents’ personality traits and the daughter’s personality or psychopathology. Moreover, correlational analysis does not define a direction for these relationships. Nevertheless, some of the parental personality traits were specific to eating-disordered daughters, suggesting that they may be relevant.
Second, I in no way believe that parents cause eating disorders (just want to make that clear before I get any attacking comments). I do think that parental personalities are significant, though. Not only do they affect your core beliefs but they also influence the relationships that you have with your parents… which affect all of your other relationships in life.
So, with that said, on to my commentary of the article!
The study used several scales (the Clinical Global Impression Scale, Beck Depression Inventory, Temperament and Character Inventory, and the Eating Disorders Inventory-2) to assess personality and ED symptomology in daughters and their parents. Among these variables were BMI, overall functioning, disease duration, eating attitudes and severity of ED behaviors, depression, and temperament. The Temperament and Character Inventory (TCI) was a large part of the study, and previous to this article I was largely unfamiliar with it, so I’ll briefly explain it at the end of the post.
In short, the personality of parents, personality of daughters, and ED symptoms were all analyzed. Among the results, some of the more interesting were:
- In AN-R, father’s persistence predicted the daughter’s age of ED onset.
- Also in AN-R, novelty-seeking, body dissatisfaction, and interpersonal distrust were all affected by the father’s reward dependence.
- Mother’s self-directedness affected novelty-seeking in AN-P and BN. The same was not true for AN-R.
- AN-P exhibited the most severe eating psychopathology. These girls had the greatest body dissatisfaction, drive to thinness, and level of depression.
- Women with AN-R were less concerned about body shape than both AN-P and BN.
- The father plays a larger role in personality-based family dynamics of ED women (especially with AN-R).
There are a MANY more conclusions than just those in the study, but I could probably write a whole series on the findings. I’m trying not to do that. There are a couple more things that I want to mention, though. First, the paper discusses the personality types of the ED-daughters. If you are a family member and are feeling attacked by this point, you might want to read this section since it’s not very complimentary to those with EDs, either. No one escapes the article feeling good:
Restricting Anorexics – stubborn, obsessive, self-determined
Purging Anorexics – impulsive, immature, disordered personalities
Bulimics – explorative, disorderly, conflicting
All EDs – frightened by potentially harmful stimuli, immature character, low self-acceptance, low resourcefulness, low self-esteem
Now, what’s the take-home message from all of this? Well, I think that the article does a good job of explaining the role of family therapy in the treatment of eating disorders. Specifically:
Counseling or family therapy may help modify specific aspects of the parent-daughter relationship to produce specific changes in eating symptoms.
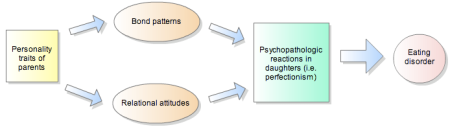
I like the point about helping the parents in family therapy. To change your relationship and your home environment, you have to help your parents. The things that you learn from them are reflections of both their own core values and their personality traits. When they are struggling with their own anxiety, negative body image, etc,., that translates. I think that when you (the person with the eating disorder) is in therapy and are being told things like it’s important to take care of yourself, you have to cut yourself some slack, what you think and how you feel matters, you don’t have to listen to the messages of society, etc., that it’s hard to believe these things and take them as truth when the people around you don’t. Will my dad ever work on his anger issues? Probably not. Do I think it would help both him and I? Sure. Is my mom ever going to let go of her own disordered eating tendencies? Unlikely. Would her being healthy being a good influence on me? Yes.
There is clearly a link between parental personality, the daughter’s personality, and ED symptoms. I think that family therapy that helps the parents with their own issues then allows them to form healthier relationships with their daughters, which helps with her ED recovery.
——————————–
The Temperament and Character Inventory (TCI)
Purpose: Instrument used for the dimensional assessment of personality, with four dimensions assessing temperament and three assessing character.
Temperament:
- Novelty seeking – level of exploratory activity
- Harm avoidance – efficacy of behavioral inhibition system
- Reward dependence – maintenance of rewarded behavior
- Persistence – ability to resist frustration
Character:
- Self-directedness – view self as autonomous and integrated
- Cooperativeness – view self as part of society
- Self-transcendence – how self is integral part of the universe
Tags:Anorexia, anorexic, anxiety, beck depression inventory, bulimia, bulimic, character, clinical global impression scale, depression, eating disorder, eating disorder symptoms, eating disorders inventory-2, family therapy, journal article, mental health, mental illness, parents, personality, psychology, psychopathology, purging anorexia, recovery, restricting, restricting anorexia, temperament and character inventory, therapy, treatment
Posted in Anorexia, Article, bulimia, treatment | 6 Comments »

 There have been
There have been  Food rituals are pretty common among individuals with eating disorders… cutting things into tiny pieces, chewing a certain number of time, mixing weird things, eating everything separate, picking food apart, etc. I’ll be the first to admit that I’ve never been terribly successful in eliminating my own food rituals. As I was miserably failing my goal to “eat a bagel normally” this morning, I was thinking about what it was that seemed so necessary about the rituals.
Food rituals are pretty common among individuals with eating disorders… cutting things into tiny pieces, chewing a certain number of time, mixing weird things, eating everything separate, picking food apart, etc. I’ll be the first to admit that I’ve never been terribly successful in eliminating my own food rituals. As I was miserably failing my goal to “eat a bagel normally” this morning, I was thinking about what it was that seemed so necessary about the rituals.