Posts Tagged ‘ptsd’
May 25, 2009
I started this day in a panic over insurance. I hate insurance. I know that is such a blind, ignorant statement, but at this moment (and a lot of other moments) I really do.
Unfortunately it is a holiday (well, that in itself is not unfortunate), which means that neither insurance nor my treatment provider is working. There’s nothing I can do about it today. I can’t resubmit my claim or beg for more days. I don’t know if I will be going to my appointment tomorrow.
I don’t want to spend the next 24+ hours fretting over this, but at the same time, I do want to. I know that worrying is not productive, but my mind is filled with “what if?”s and worst-case scenarios. It’s as if turning it over and over in my mind will somehow prepare me for whatever happens tomorrow.
While trying to remind myself that worrying is not productive, I remembered this quote:
Behind all of this lay the “mind like water” concept … when you throw a pebble into a pond, what does the water do? It responds with total appropriateness to the force and mass of the rock. It does nothing more and nothing less. It doesn’t overreact or underreact. It doesn’t react at all. It simply interacts with whatever comes to it and then returns to its natural state. – David Allen, Getting Things Done
So that’s my goal for today and tomorrow: “mind like water.” I have to let it go for today. I will try and be calm until hit with the insurance rocks.
Tags:Anorexia, anorexic, anxiety, bulimia, bulimic, david allen, depression, eating disorder, getting things done, health insurance, insurance, mental health, mental illness, psychology, ptsd
Posted in anxiety, mental health, therapy, treatment | 2 Comments »
May 18, 2009
 There have been many blog posts written on facebook and pro-anorexia, however, lately I’ve been thinking a lot about facebook and recovery in general.
There have been many blog posts written on facebook and pro-anorexia, however, lately I’ve been thinking a lot about facebook and recovery in general.
Facebook is really unique in that EVERYONE (okay, almost everyone) is on it. If you’re an eating disorder patient, this means your professionals, the other girls/guys you’re in treatment with, past patients, your school / work friends who may not know about your eating disorder, your family members, etc. In what other realm do all of these people connect?
For most people, “Facebook stalking” means checking out what that guy you liked in high school is doing now (or some variation of that idea). However, for anyone in eating disorder treatment, Facebook stalking can mean following up on the girls you were in treatment with or tracking down all of the professionals you’ve worked with.
Luckily, there are privacy settings. Some professionals even know how to use them.
I was pretty convinced that facebook could be nothing but hurtful to recovery until a girl I used to be in treatment with told me how she and another woman used it to keep in touch. There’s probably a 20-year age difference between the two girls (for the sake of this example, let’s call the older one Kristy and the younger one Jackie), but neither of them had a lot of support outside of their families. In the evenings they would talk on facebook (something I haven’t gotten into yet — facebook messenger). Kristy would see the unhealthy things about dieting that girls would post on Jackie’s wall, with prom coming up, and they’d talk about it. Jackie saw all the cute pictures of Kristy’s kids. Basically, it served as an outlet for both of them — something that was missing in their outside world.
Now, you could argue that this isn’t different than email or IM, but I don’t think that IM bridged the age-barrier in the same way that facebook is now. IM also doesn’t have the public information that facebook has — you can’t see how others interact with someone.
So what do you think about facebook — helpful or harmful to recovery? Staying in touch with people you were residential with could definitely be triggering (especially if they are not doing well and you have access to their photos), but having the support of people who have been great friends is also valuable. And I’d love to know — do professionals ever search for their clients on facebook? Just out of curiosity? For the record, I have never tried to friend a professional myself — although I won’t lie, I have looked at a couple of profiles.
Tags:Anorexia, anorexic, anxiety, blog post, bulimia, bulimic, depression, Dieting, eating disorder, eating disorder treatment, facebook, facebook stalking, inpatient, mental health, mental illness, pro-anorexia, professionals, psychiatry, psychology, ptsd, recovery, relapse, relationships, residential, social media, therapist, trauma, treatment, triggering
Posted in eating disorder, online support, relationships | 14 Comments »
March 17, 2009
I stumbled upon this article last week: Metabolic Assessment of Menstruating and Nonmenstruating Normal Weight Adolescents This is something that I have always been curious about — is amenorrhea associated with a low metabolic rate? I always assumed yes, at least a little bit. However, I didn’t really base this conclusion on any hard science. Let’s say that I used “Grey Science,” which goes something like this:
Your body requires a certain number of calories to function at full-capacity. When you chronically deprive your body of these calories, it has to adapt to the calorie deficit to survive. One of the ways that it does this is to cut out non-essential functions, like menstruation. However, in recovery, it’s possible to gain weight without really restoring your metabolism (believe me). If you’re still subsisting on a sub-optimal number of calories, then your body might still not feel like it can spare the extra calories that menstruation requires. You are only able to maintain that weight on those calories because there are still processes that are being cut out. This means that your metabolic rate is lower.
Again, this is my unscientific reason, that happens to make a lot of sense in my mind. Thankfully some researchers came along to actually research this…
From the article:
“The purpose of this study was to investigate a possible mechanism for amenorrhea in adolescents who were 90-130% expected body weight with a history of anorexia nervosa, bulimia nervosa, or eating disorder not otherwise specified. Using indirect calorimetry, we examined the metabolic differences between participants who were menstruating regularly compared with those who were amenorrheic. Our hypothesis was that participants with amenorrhea would have a lower REE than those with regular menses. We also proposed that both groups would have a lower REE than would be expected for age, weight, and height due to their dieting, calorie restriction, and eating disorder behaviors.”
And the conclusion:
“Using indirect calorimetry to assess REE, we showed that a hypometabolic state persists despite weight restoration. There were significant metabolic differences found in weight-restored participants was amenorrhea as compared to participants who had regular menses. Participants with amenorrhea consumed a lower fat diet, that a lower REE, and were at a lower mean body weight.”
So… overall, I was on the right track. However, the article leaves me with several questions:
- Why do recovered anorexics/bulimics have a lower REE than others their age without an ED history?
- What is necessary for resuming menses?
- I have been told by several doctors that often a stint on birth control is necessary to “jump-start” your period. How does that relate? And, how does that affect REE?
I think that the situation is a Catch-22. Weight-restored patients with amenorrhea have a lower REE, so their metabolic rate is reduced and therefore need fewer calories. However, they are still not getting their period, so do they need to be eating more? I understand that you need to eat more to raise your metabolic rate and get your period back (in theory), but as a weight-restored anorexic I will tell you that my ED is screaming, “See! You DON’T need that much food! Your metabolism is slower!” I think that it is a particularly difficult spot to be in since you can’t tell yourself “Well, you do need to gain…” I am waiting for a follow-up study that shows that increasing caloric intake fixes said metabolic and menstrual issues. Now THAT is a study I would be excited to read.
(Unrelated P.S. – This is the 100th Grey Thinking post!)
Tags:amenorrhea, Anorexia, anorexic, anxiety, bulimic, depression, eating disorder, ED, ED treatment, menstrual problems, mental health, mental illness, metabolic rate, metabolism, psychology, ptsd, recovery, treatment, weight gain
Posted in Anorexia, bulimia, eating disorder | 8 Comments »
July 7, 2008
I have just been waiting to write about this article all day!
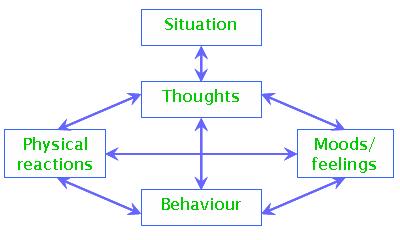
Cognitive Behavioral Therapy
“The [UK] government has earmarked £173m to increase the number of cognitive behavioural therapists in the NHS.””Professor Mick Cooper, an expert in counselling at the University of Strathclyde, told the conference at the University of East Anglia that although he welcomed the increased funding for psychological therapies, the focus on CBT was not logical.
He and three colleagues from the UK and US issued a statement saying there had been more studies on CBT, but that did not necessarily mean it was more effective than other types of therapy.
“It is scientifically irresponsible to continue to imply and act as though CBTs are more effective, as has been done in justifying the expenditure of £173m to train CBT therapists throughout England.
“Such claims harm the public by restricting patient choice and discourage some psychologically distressed people from seeking treatment,” he said.”
- This argument reminds me of my Dr. Drew Westen grad seminar days… Everyone is using CBT because it’s the easiest to research, has the most funding, etc. etc. Can’t say that I disagree — there is definitely too much hype about CBT. However, I don’t think that most professionals follow CBT guidelines even 75% of the time — it’s just not practical! Dr. Cooper has a great explanation of this:
“What is more, where researchers have allegiances to one particular approach, the control ‘therapies’ that are developed to test these approaches against often bear little relationship to those approaches as actually practiced in the field, and cannot really be considered therapeutic at all (Wampold, 2001, p.104) (Shapiro and Shapiro (1982) refer to these approaches as ‘straw men’). In the Foa et al. (1991) study of PTSD in women who had been raped, for instance, therapists in the ‘supportive counselling’ condition were instructed that, if their clients started to talk about their assault, they should redirect them to focus on current daily problems! “
Every therapist is going to respond similarly to some extent… maybe one is going to focus on though restructuring more than childhood, but you’re still going to have that consoling feeling. I think that whatever this common feeling is makes up the healing component of therapy… which is why the best predictor of treatment outcome is therapeutic alliance. This common set of elements that spans the different types of therapies has been termed the ‘Dodo bird’ verdict. I’ll have to write a post on that later…
Anyway, it’s nice to see someone arguing against CBT for a change! The world (and psych field) could use a little more psychoanalysis 🙂
Technorati Tags:
eating disorders, anorexia, bulimia, CBT, talk therapy, psychotherapy, therapist, psychology, psychoanalysis, NHS, psych research, treatment, mental illness, mental health, Dodo bird
Tags:Anorexia, anxiety, bulimia, CBT, depression, Dodo bird, eating disorders, mental health, mental illness, NHS, psych research, psychoanalysis, psychology, psychotherapy, ptsd, talk therapy, therapist, treatment
Posted in Article, Pop Psych, therapy | 7 Comments »
July 7, 2008
I have just been waiting to write about this article all day!
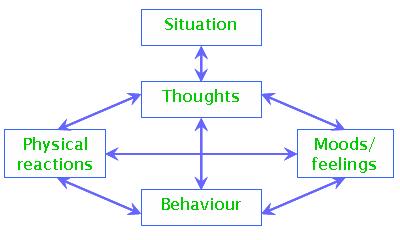
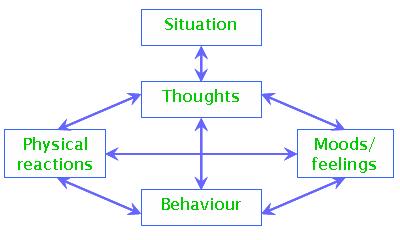
Cognitive Behavioral Therapy
“The [UK] government has earmarked £173m to increase the number of cognitive behavioural therapists in the NHS.””Professor Mick Cooper, an expert in counselling at the University of Strathclyde, told the conference at the University of East Anglia that although he welcomed the increased funding for psychological therapies, the focus on CBT was not logical.
He and three colleagues from the UK and US issued a statement saying there had been more studies on CBT, but that did not necessarily mean it was more effective than other types of therapy.
“It is scientifically irresponsible to continue to imply and act as though CBTs are more effective, as has been done in justifying the expenditure of £173m to train CBT therapists throughout England.
“Such claims harm the public by restricting patient choice and discourage some psychologically distressed people from seeking treatment,” he said.”
- This argument reminds me of my Dr. Drew Westen grad seminar days… Everyone is using CBT because it’s the easiest to research, has the most funding, etc. etc. Can’t say that I disagree — there is definitely too much hype about CBT. However, I don’t think that most professionals follow CBT guidelines even 75% of the time — it’s just not practical! Dr. Cooper has a great explanation of this:
“What is more, where researchers have allegiances to one particular approach, the control ‘therapies’ that are developed to test these approaches against often bear little relationship to those approaches as actually practiced in the field, and cannot really be considered therapeutic at all (Wampold, 2001, p.104) (Shapiro and Shapiro (1982) refer to these approaches as ‘straw men’). In the Foa et al. (1991) study of PTSD in women who had been raped, for instance, therapists in the ‘supportive counselling’ condition were instructed that, if their clients started to talk about their assault, they should redirect them to focus on current daily problems! “
Every therapist is going to respond similarly to some extent… maybe one is going to focus on though restructuring more than childhood, but you’re still going to have that consoling feeling. I think that whatever this common feeling is makes up the healing component of therapy… which is why the best predictor of treatment outcome is therapeutic alliance. This common set of elements that spans the different types of therapies has been termed the ‘Dodo bird’ verdict. I’ll have to write a post on that later…
Anyway, it’s nice to see someone arguing against CBT for a change! The world (and psych field) could use a little more psychoanalysis 🙂
Technorati Tags:
eating disorders, anorexia, bulimia, CBT, talk therapy, psychotherapy, therapist, psychology, psychoanalysis, NHS, psych research, treatment, mental illness, mental health, Dodo bird
Tags:Anorexia, anxiety, bulimia, CBT, depression, Dodo bird, eating disorders, mental health, mental illness, NHS, psych research, psychoanalysis, psychology, psychotherapy, ptsd, talk therapy, therapist, treatment
Posted in Article, Pop Psych, therapy | 7 Comments »
June 28, 2008
Group Therapy May Help Memory
“Memory lapses could initially be caused by psychological stress. If the memory lapses are noticed, they can lead to anger and fear. Ultimately, this leads to heightened stress levels, which in turn increase the risk of memory lapses. This vicious circle capturing the sufferers is best characterized by models of somatoform disorders.”
So many studies (of different populations) have proven group therapy to be helpful: cancer survivor groups, alcoholics anonymous, grief & lost groups… there is definitely a lot to be said about sharing your feelings, relating to the experiences of others, getting advice, and giving some back.
I thought this article was interesting because of the direct connection between memory and mental illness…
stressor –> anger and fear –> heightened stress levels –> memory impairment
This isn’t really anything new… really post PTSD literature will tell you the same thing. You experience a traumatic event, it is too stressful (stressful can meaning scary, hurtful, etc.) for you to be able to handle/comprehend. You repress (or suppress — that’s another discussion in itself) the memory, but unconsciously/subconsciously it still bothers you. This distraction results in decreased memory function.
The biggest advantage of group therapy? Relating to others’ experiences and understanding more of your own. The biggest disadvantage? The trigger of these relatable experiences and the reliving of your own.
I’ve never been in an ED group that allowed talk about trauma. Even in the trauma groups I’ve been to, details of everyone’s stories have always vague. That’s pretty counterproductive, now that I think about it… discouraging talk about already isolating and taboo subjects… but there was some common understanding that sharing experiences with others could be a bad thing — you don’t want to bring up more trauma issues for anyone. You have to be careful.
I’m not sure how I really feel about those groups or that whole concept, and memory disturbance-causing stressors are probably rarely traumatic events… but how ironic that this treatment proposal is exactly what we were told not to do.
This is the same relationship between my ED treatment experiences and the Maudsley approach. I was always told that it’s not about the food — if you’re talking about the food, then you’re concentrating on that because it’s easier to obsess over that than to deal with more painful emotions. Not that Maudsley doesn’t involve any therapy (not making that assertion at all), but it strikes me as very “yes it IS about the food.”
I definitely keep up on psych research more than anyone I know… but it kinda makes you lose faith in the field. So much is contradictory… it’s not a hard science, so we don’t really know what works.
Maybe you can argue that treatment can be whatever you want it to be (you can definitely argue that different people require different kinds of treatment). I really believe that there has to be some more systematic approach to handling mental illness, though.
Tags:Anorexia, bulimia, eating disorder, eating disorder treatment, group therapy, Maudsley, memory impairment, psych research, ptsd, somatoform disorders, therapy, trauma
Posted in Article, eating disorder, ptsd | 1 Comment »
March 19, 2008
While I was really excited upon seeing this study, it left me with more questions than answers.
The finding that traumatic events can actually alter a stress-related gene is definitely a new idea. However, it has been believed for years that these significant events cause some neurological change. Previously, researchers have found:
1. In a study by Martin Teicher at McLean Hospital, boys who were neglected also had a smaller corpus collosum. The same was true for girls who were sexually abused. Teicher explains that “We believe that a smaller corpus collosum leads to less integration of the two halves of the brain, and that this can result in dramatic shifts in mood and personality.”
2. Patients with a history of sexual or verbal abuse show less blood flow in the cerebellar vermis — a part of the brain that helps with the maintenance of emotional balance. According to Teicher, the vermis is strongly influenced by the environment as opposed to genetic factors.
3. Stress hormones released by abuse affect the brain’s ability to receive and send signals. In this way, the brain is “rewired” to overrespond to stress — increasing fear, anxiety, and the fight-or-flight reaction.
These are just a few examples. So, discovering that there is a stress gene definitely supports the argument that mental health has a biological component, but it leaves us with the same questions.
1. How do people with the PTSD-prone variation of the stress gene who don’t encounter a traumatic event react to other stress? Do they still overrespond?
2. Why are symptoms not manifested until years after the event?
3. Is the stress gene only impressionable during childhood?
4. Do medication and therapy re-regulate the gene? Or just treat the symptoms?
… personally, I am waiting for the therapy gene – the gene that determines who will / will not respond to therapy 🙂
Tags:biological psychology, depression, ptsd, stress disorder, stress gene
Posted in Article, depression, Pop Psych, ptsd | Leave a Comment »
 There have been
There have been