There have been many studies on family dynamics and the development of eating disorders, but I think that this is the first that I’ve seen that takes the next step and makes connections with specific symptomology: The dynamic relationship of parental personality traits with the personality and psychopathology traits of anorectic and bulimic daughters
Before I go further, I want to make two disclaimers. First, from the article:
…we cannot infer a casual relationship between the parents’ personality traits and the daughter’s personality or psychopathology. Moreover, correlational analysis does not define a direction for these relationships. Nevertheless, some of the parental personality traits were specific to eating-disordered daughters, suggesting that they may be relevant.
Second, I in no way believe that parents cause eating disorders (just want to make that clear before I get any attacking comments). I do think that parental personalities are significant, though. Not only do they affect your core beliefs but they also influence the relationships that you have with your parents… which affect all of your other relationships in life.
So, with that said, on to my commentary of the article!
The study used several scales (the Clinical Global Impression Scale, Beck Depression Inventory, Temperament and Character Inventory, and the Eating Disorders Inventory-2) to assess personality and ED symptomology in daughters and their parents. Among these variables were BMI, overall functioning, disease duration, eating attitudes and severity of ED behaviors, depression, and temperament. The Temperament and Character Inventory (TCI) was a large part of the study, and previous to this article I was largely unfamiliar with it, so I’ll briefly explain it at the end of the post.
In short, the personality of parents, personality of daughters, and ED symptoms were all analyzed. Among the results, some of the more interesting were:
- In AN-R, father’s persistence predicted the daughter’s age of ED onset.
- Also in AN-R, novelty-seeking, body dissatisfaction, and interpersonal distrust were all affected by the father’s reward dependence.
- Mother’s self-directedness affected novelty-seeking in AN-P and BN. The same was not true for AN-R.
- AN-P exhibited the most severe eating psychopathology. These girls had the greatest body dissatisfaction, drive to thinness, and level of depression.
- Women with AN-R were less concerned about body shape than both AN-P and BN.
- The father plays a larger role in personality-based family dynamics of ED women (especially with AN-R).
There are a MANY more conclusions than just those in the study, but I could probably write a whole series on the findings. I’m trying not to do that. There are a couple more things that I want to mention, though. First, the paper discusses the personality types of the ED-daughters. If you are a family member and are feeling attacked by this point, you might want to read this section since it’s not very complimentary to those with EDs, either. No one escapes the article feeling good:
Restricting Anorexics – stubborn, obsessive, self-determined
Purging Anorexics – impulsive, immature, disordered personalities
Bulimics – explorative, disorderly, conflicting
All EDs – frightened by potentially harmful stimuli, immature character, low self-acceptance, low resourcefulness, low self-esteem
Now, what’s the take-home message from all of this? Well, I think that the article does a good job of explaining the role of family therapy in the treatment of eating disorders. Specifically:
Counseling or family therapy may help modify specific aspects of the parent-daughter relationship to produce specific changes in eating symptoms.
I like the point about helping the parents in family therapy. To change your relationship and your home environment, you have to help your parents. The things that you learn from them are reflections of both their own core values and their personality traits. When they are struggling with their own anxiety, negative body image, etc,., that translates. I think that when you (the person with the eating disorder) is in therapy and are being told things like it’s important to take care of yourself, you have to cut yourself some slack, what you think and how you feel matters, you don’t have to listen to the messages of society, etc., that it’s hard to believe these things and take them as truth when the people around you don’t. Will my dad ever work on his anger issues? Probably not. Do I think it would help both him and I? Sure. Is my mom ever going to let go of her own disordered eating tendencies? Unlikely. Would her being healthy being a good influence on me? Yes.
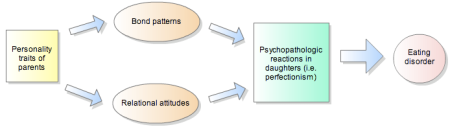
There is clearly a link between parental personality, the daughter’s personality, and ED symptoms. I think that family therapy that helps the parents with their own issues then allows them to form healthier relationships with their daughters, which helps with her ED recovery.
——————————–
The Temperament and Character Inventory (TCI)
Purpose: Instrument used for the dimensional assessment of personality, with four dimensions assessing temperament and three assessing character.
Temperament:
- Novelty seeking – level of exploratory activity
- Harm avoidance – efficacy of behavioral inhibition system
- Reward dependence – maintenance of rewarded behavior
- Persistence – ability to resist frustration
Character:
- Self-directedness – view self as autonomous and integrated
- Cooperativeness – view self as part of society
- Self-transcendence – how self is integral part of the universe

 Once in awhile, my therapist assigns me homework — usually for one of several reasons:
Once in awhile, my therapist assigns me homework — usually for one of several reasons: